Great Health Great Fitness
“The Courageous Battle: Understanding Lupus and Navigating Its Challenges”
Enter the battlefield of understanding with 'The Courageous Battle: Understanding Lupus and Navigating Its Challenges.' Explore the complexities of this chronic autoimmune warrior, discovering resilience amidst its trials. Uncover the strength within to navigate the twists and turns of this formidable opponent, forging a path toward wellness and empowerment.
Introduction to Lupus:
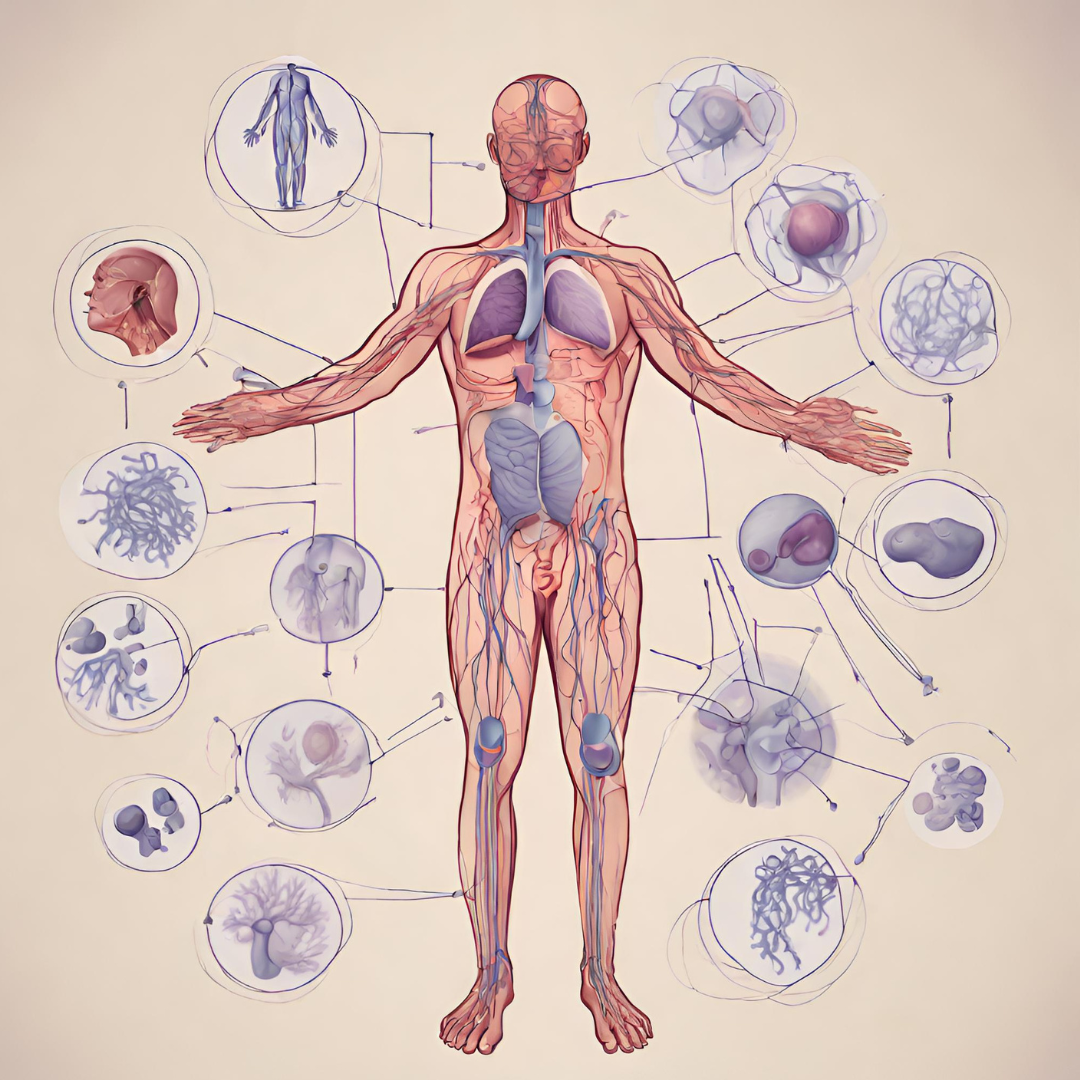
Lupus is a chronic autoimmune disease that can affect various parts of the body, including the skin, joints, kidneys, heart, lungs, brain, and blood cells. It occurs when the immune system attacks healthy tissues and organs, leading to inflammation, pain, and damage. It is a complex and often misunderstood condition, affecting individuals of all ages, genders, and ethnicities. In this comprehensive guide, we will delve into the various aspects of lupus, from its causes and symptoms to diagnosis, treatment options, and strategies for living well with the disease.
Understanding the Basics of Lupus:
To understand this, it’s essential to grasp the fundamentals of autoimmune diseases and how they manifest in the body. We’ll explore the underlying mechanisms of this, including genetic factors, environmental triggers, and dysregulation of the immune system. From there, we’ll delve into the different types of lupus, including systemic lupus erythematosus (SLE), discoid lupus erythematosus (DLE), subacute cutaneous lupus erythematosus (SCLE), and others, each with its own set of symptoms and complications.
Signs and Symptoms of Lupus:

It is known for its wide range of symptoms, which can vary in severity and fluctuate over time. From fatigue and joint pain to skin rashes and organ involvement, we’ll explore the common signs and symptoms of lupus, as well as less common manifestations that may present challenges in diagnosis. Additionally, we’ll discuss the importance of recognizing lupus flares, periods of increased disease activity, and how to manage symptoms effectively.
- Fatigue:
- Persistent and debilitating fatigue is one of the hallmark symptoms of this, often described as overwhelming and unrelenting despite rest.
- Joint Pain and Swelling:
- It can cause inflammation in the joints, leading to pain, stiffness, and swelling. Joint involvement may be symmetric and affect multiple joints, such as the fingers, wrists, knees, and ankles.
- Skin Rash:
- A characteristic rash known as a “butterfly rash” may develop on the face, spanning across the cheeks and nose in a butterfly-wing pattern. Other skin manifestations of lupus include discoid lesions, photosensitivity (increased sensitivity to sunlight), and mucosal ulcers.
- Fever:
- Low-grade fevers or recurrent episodes of fever may occur in individuals with , often accompanied by fatigue and malaise.
- Raynaud’s Phenomenon:
- Raynaud’s phenomenon is a condition characterized by abnormal blood vessel spasms in response to cold or stress, leading to color changes in the fingers and toes, such as pallor, followed by cyanosis (blueness) and redness.
- Hair Loss:
- Hair loss or thinning, known as alopecia, may occur in individuals, affecting the scalp, eyebrows, eyelashes, or other body areas.
- Oral and Nasal Ulcers:
- Mouth sores (oral ulcers) and nasal ulcers may develop in some individuals with lupus, causing pain and discomfort.
- Chest Pain:
- It can affect the heart and lungs, leading to chest pain, palpitations, shortness of breath, and pleurisy (inflammation of the lining of the lungs).
- Kidney Problems:
- The nephritis, inflammation of the kidneys, is a serious complication that can cause proteinuria (protein in the urine), hematuria (blood in the urine), edema (swelling), and hypertension.
- Neurological Symptoms:
- It can affect the nervous system, causing symptoms such as headaches, cognitive dysfunction (brain fog), seizures, mood changes, and peripheral neuropathy (nerve damage).
- Gastrointestinal Symptoms:
- Digestive issues, including abdominal pain, nausea, vomiting, diarrhea, and loss of appetite, may occur in individuals with lupus.
- Eye Problems:
- It can affect the eyes, leading to dry eyes, blurred vision, eye pain, and, in severe cases, retinal vasculitis or optic neuritis.
Diagnosing Lupus:
Diagnosing it can be challenging, as it often mimics other conditions and varies greatly from person to person. We’ll examine the diagnostic criteria for established by the American College of Rheumatology (ACR) and discuss the role of medical history, physical examination, laboratory tests, and imaging studies in confirming a diagnosis. Early detection and accurate diagnosis are crucial for initiating timely treatment and preventing long-term complications.
Treatment Approaches for Lupus:
While there is no cure for disease, various treatment options are available to manage symptoms, reduce inflammation, and prevent disease flares. We’ll explore the different categories of medications commonly used to treat lupus, including nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, antimalarial drugs, immunosuppressants, and biologic agents. Additionally, we’ll discuss complementary and alternative therapies, lifestyle modifications, and self-care strategies that can complement conventional treatment approaches.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs):
- NSAIDs, such as ibuprofen and naproxen, can help alleviate pain, inflammation, and fever associated with lupus. They are often used to manage mild to moderate joint pain and musculoskeletal symptoms.
- Corticosteroids:
- Corticosteroids, such as prednisone or prednisolone, are powerful anti-inflammatory medications that can effectively control lupus flares and suppress immune activity. They may be prescribed in low to high doses, depending on disease severity and organ involvement.
- Antimalarial Drugs:
- Antimalarial medications, such as hydroxychloroquine (Plaquenil) and chloroquine, are commonly used to treat lupus skin rashes, joint pain, and fatigue. They have anti-inflammatory and immunomodulatory properties and are often prescribed as long-term maintenance therapy.
- Immunosuppressants:
- Immunosuppressive drugs, including methotrexate, azathioprine, mycophenolate mofetil, and cyclophosphamide, may be used to suppress overactive immune responses and reduce inflammation in individuals with more severe or organ-threatening lupus manifestations, such as nephritis or central nervous system involvement.
- Biologic Therapies:
- Biologic medications, such as belimumab (Benlysta), target specific components of the immune system involved in the pathogenesis of lupus. Belimumab, the first FDA-approved biologic therapy for this, is indicated for the treatment of active systemic lupus erythematosus (SLE) in certain patients.
- Topical Treatments:
- Topical medications, such as corticosteroid creams, ointments, or gels, may be used to manage localized lupus skin rashes, discoid lesions, or mucosal ulcers.
- Complementary and Alternative Therapies:
- Complementary and alternative therapies, such as acupuncture, massage therapy, yoga, and dietary supplements, may be incorporated into the treatment plan to help manage symptoms, improve overall well-being, and enhance quality of life. However, it’s essential to discuss these therapies with a healthcare professional to ensure safety and effectiveness.
- Lifestyle Modifications:
- Lifestyle modifications, including maintaining a balanced diet, getting regular exercise, managing stress, avoiding smoking, limiting alcohol intake, and practicing sun protection, are essential for managing lupus and promoting overall health.
- Monitoring and Follow-Up Care:
- Regular monitoring and follow-up care with healthcare providers, including rheumatologists, nephrologists, dermatologists, and other specialists, are crucial for assessing disease activity, monitoring medication side effects, adjusting treatment regimens as needed, and addressing emerging symptoms or complications.
- Patient Education and Support:
- Patient education and support programs, such as support groups, educational materials, and online resources, can provide valuable information, emotional support, and practical strategies for coping with this and navigating the challenges of living with a chronic illness.
Living Well with Lupus:
Managing this goes beyond medical treatment—it requires a holistic approach that addresses physical, emotional, and social well-being. We’ll provide practical tips and strategies for living well with disease, including maintaining a healthy lifestyle, managing stress, getting regular exercise, prioritizing sleep, and seeking support from healthcare providers, family, and friends. Additionally, we’ll address common challenges faced by individuals with lupus, such as navigating relationships, employment, and financial concerns, and offer guidance on overcoming obstacles and building resilience.
Research and Advancements in Lupus:
Advancements in research and treatment have improved our understanding of lupus and expanded treatment options for individuals living with the disease. We’ll explore recent developments in research, including emerging therapies, biomarkers for disease activity and progression, and efforts to improve diagnosis and personalized treatment approaches. Additionally, we’ll discuss the importance of advocacy and participation in clinical trials to drive progress in research and improve outcomes for future generations.
- Improved Understanding of Lupus Pathogenesis:
- Researchers have made significant strides in unraveling the complex mechanisms underlying , including aberrant immune responses, genetic predisposition, environmental triggers, and dysregulation of immune signaling pathways. Advances in genomic and molecular studies have provided insights into the genetic basis of lupus susceptibility and identified potential targets for therapeutic intervention.
- Biomarkers for Disease Activity and Progression:
- Biomarkers are biological indicators that can provide valuable information about disease activity, severity, and response to treatment. Efforts to identify reliable biomarkers are ongoing, with a focus on markers of inflammation, immune activation, organ involvement, and treatment response. Biomarker discovery holds promise for improving disease monitoring, guiding treatment decisions, and predicting long-term outcomes in lupus patients.
- Targeted Therapies and Biologic Agents:
- The development of targeted therapies and biologic agents has revolutionized the treatment of this, offering new options for individuals with refractory or severe disease. Biologic medications, such as belimumab (Benlysta), rituximab, and other monoclonal antibodies, target specific components of the immune system involved in pathogenesis. These therapies have demonstrated efficacy in reducing disease activity, preventing flares, and improving quality of life for some patients.
- Personalized Medicine Approaches:
- Personalized medicine approaches aim to tailor treatment regimens to individual patient characteristics, including genetic background, disease phenotype, biomarker profiles, and treatment response. By stratifying lupus patients into subgroups based on distinct molecular signatures or clinical features, personalized medicine approaches may optimize treatment outcomes, minimize adverse effects, and enhance therapeutic efficacy.
- Clinical Trials and Drug Development:
- Clinical trials play a critical role in evaluating the safety and efficacy of new therapies and advancing the standard of care for patients. Pharmaceutical companies, academic institutions, and government agencies are actively conducting clinical trials to test novel drug candidates, assess combination therapies, and explore innovative treatment approaches. Participation in clinical trials offers patients access to cutting-edge therapies and contributes to the advancement of research.
- Patient-Centered Outcomes Research:
- Patient-centered outcomes research focuses on understanding the lived experiences of individuals with lupus, identifying unmet needs, and incorporating patient perspectives into research priorities and clinical care. Engaging patients as partners in research, advocacy, and decision-making empowers individuals with disease to actively participate in their care, advocate for their needs, and contribute to research efforts aimed at improving outcomes and quality of life.
- Advances in Technology and Data Science:
- Advances in technology, including high-throughput sequencing, omics technologies, bioinformatics, and computational modeling, have accelerated progress in research by enabling large-scale data analysis, identification of disease-related pathways, and drug discovery. Big data analytics, machine learning algorithms, and artificial intelligence tools hold promise for uncovering novel insights into lupus pathogenesis, predicting disease outcomes, and optimizing treatment strategies.
- International Collaborative Initiatives:
- International collaborative initiatives, such as the Lupus Foundation of America (LFA) Collective Data Analysis Initiative, the Systemic Lupus International Collaborating Clinics (SLICC) network, and the Lupus Research Alliance (LRA) Lupus Clinical Investigators Network (LuCIN), foster collaboration among researchers, clinicians, patient advocates, and industry partners to accelerate progress in research, standardize clinical assessment tools, and facilitate data sharing and dissemination.
- Patient Engagement and Advocacy:
- Patient engagement and advocacy efforts play a vital role in driving research, raising awareness, and mobilizing resources to support research initiatives. Patient advocacy organizations, such as the Lupus Foundation of America (LFA), the Lupus Research Alliance (LRA), and the Lupus UK, advocate for increased funding, policy changes, and public awareness campaigns to address the unmet needs of the lupus community and improve access to care and treatments.
- Emerging Therapeutic Targets and Strategies:
- Emerging therapeutic targets and strategies are being explored to address the complex and heterogeneous nature of lupus and overcome treatment resistance. Research efforts are focused on modulating immune checkpoints, targeting cytokines and inflammatory mediators, restoring immune tolerance, and promoting tissue repair and regeneration. Novel therapeutic modalities, such as gene therapy, cell-based therapies, and small molecule inhibitors, are under investigation for their potential to revolutionize lupus treatment in the future.
Conclusion:
Living with this presents unique challenges, but with knowledge, support, and proactive management, individuals with lupus can lead fulfilling and meaningful lives. By understanding the complexities of lupus, advocating for optimal care, and embracing a positive mindset, individuals can navigate the challenges of the disease with courage and resilience. With ongoing research and advancements in treatment, there is hope for a brighter future for all those affected by lupus. For More Information you can check our blogs “COVID-19: The Triumph Trail – Overcoming Life After COVID-19”.
