Great Health Great Fitness
“Pneumonia: Unveiling the Hidden Threat to Health”
Beneath the surface of seemingly innocuous symptoms lies a formidable foe: pneumonia. This silent threat to health often lurks undetected until it strikes with debilitating force. By shedding light on its hidden presence, we arm ourselves with knowledge and vigilance. Let us unveil the secrets of pneumonia, empowering ourselves to recognize, prevent, and combat this stealthy adversary for the sake of our well-being.
Introduction to Pneumonia: Unraveling the Hidden Threat
Pneumonia, an insidious respiratory infection, remains a formidable challenge in global health, often underestimated in its severity and impact. This section will embark on an exhaustive exploration of pneumonia, encompassing its intricate nature, multifaceted causes, nuanced risk factors, and pervasive presence in society.
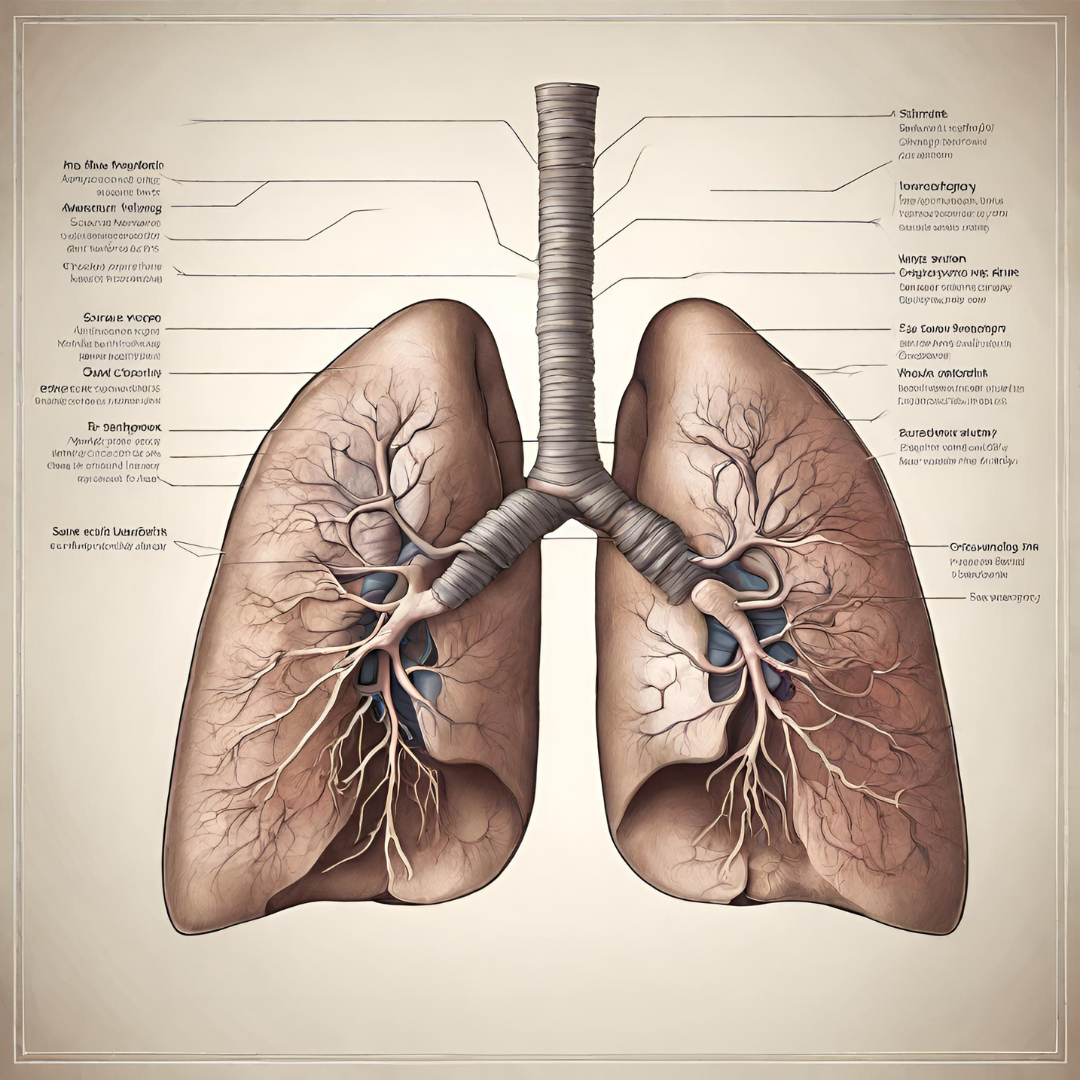
The manifests as a complex inflammatory response within the lungs, characterized by the infiltration of infectious agents and subsequent consolidation of lung tissue. Its etiology spans a diverse array of pathogens, including bacteria, viruses, fungi, and less frequently, parasites, each wielding unique mechanisms of pathogenesis. An in-depth comprehension of these microbial assailants is fundamental to unraveling the mysteries of pneumonia and devising effective countermeasures.
It impact extends beyond the individual level to affect communities, healthcare systems, and economies. The burden of pneumonia is particularly pronounced in low- and middle-income countries, where access to healthcare resources and preventive measures may be limited. By understanding the far-reaching consequences of this, policymakers, healthcare providers, and the public can mobilize efforts to mitigate its impact and improve outcomes.
Delving into the Pathophysiology of Pneumonia
The pathophysiology is a labyrinthine landscape of host-pathogen interactions, immunological skirmishes, and tissue remodeling processes. This section will navigate through the intricate mechanisms underlying pneumonia development, shedding light on the intricate dance between microbial invaders and the host’s innate and adaptive immune responses.
Upon encountering a respiratory pathogen, the immune system orchestrates a cascade of events aimed at neutralizing the threat and restoring tissue homeostasis. However, dysregulation of this immune response can lead to collateral damage, exacerbating lung injury and impairing gas exchange. An in-depth understanding of these pathophysiological intricacies is imperative for devising targeted therapeutic interventions that mitigate inflammation, promote tissue repair, and restore pulmonary function.
The pathophysiology involves a dynamic interplay between the invading pathogen and the host’s immune system. Initial recognition of the pathogen by immune cells triggers an inflammatory response, characterized by the release of cytokines and chemokines that recruit additional immune cells to the site of infection. This inflammatory cascade serves to contain and eliminate the pathogen, but unchecked inflammation can lead to tissue damage and compromise lung function.
Illuminating the Epidemiology and Burden of Pneumonia
It exacts a significant toll on global health, with a disproportionate impact on vulnerable populations and resource-limited settings. This section will illuminate the epidemiological landscape of pneumonia, charting its prevalence, incidence, and mortality across diverse demographic strata and geographic regions.
Epidemiological data unveil a stark reality: it spares no one, afflicting individuals of all ages and socioeconomic backgrounds, albeit with varying severity and outcomes. Children under five years of age, older adults, and individuals with underlying health conditions bear the brunt of wrath, facing heightened susceptibility to severe disease and adverse outcomes. Disparities in access to healthcare, vaccination coverage, and environmental factors further exacerbate the burden of pneumonia, underscoring the urgency of targeted interventions and equitable healthcare delivery.
The burden extends beyond individual health outcomes to encompass broader social and economic implications. The direct medical costs associated with treatment, including hospitalization, medications, and follow-up care, can impose a significant financial strain on healthcare systems and households alike. Indirect costs, such as lost productivity due to illness or premature death, further compound the economic burden of pneumonia, highlighting the need for comprehensive strategies to mitigate its impact.
Deciphering the Clinical Presentation and Diagnostic Dilemmas of Pneumonia
Recognizing the protean manifestations is paramount for timely diagnosis and intervention. This section will embark on a comprehensive exploration of the clinical spectrum of pneumonia, unraveling its diverse array of signs and symptoms, ranging from subtle respiratory distress to fulminant respiratory failure.
Clinical diagnosis of pneumonia poses a formidable challenge, often necessitating a multifaceted approach that integrates clinical assessment, radiological imaging, and microbiological testing. Chest X-rays, computed tomography scans, and point-of-care diagnostic tests play pivotal roles in confirming the diagnosis and elucidating the underlying etiology. However, the nuances of diagnosis extend beyond mere laboratory findings, encompassing a nuanced understanding of patient history, physical examination findings, and contextual factors that inform clinical decision-making.
The clinical presentation can vary widely depending on factors such as the underlying pathogen, the host’s immune status, and the presence of comorbidities. Common symptoms include cough, fever, dyspnea, chest pain, and sputum production, but atypical presentations, particularly in vulnerable populations such as older adults or immunocompromised individuals, can pose diagnostic challenges. By familiarizing healthcare providers with the diverse clinical manifestations of pneumonia, this section aims to enhance diagnostic accuracy and facilitate timely intervention.
Clinical Presentation:
- Respiratory Symptoms: It typically presents with symptoms such as cough, often producing sputum (which may be purulent), shortness of breath, and chest pain, especially when breathing deeply or coughing.
- Systemic Symptoms: Patients may experience systemic symptoms like fever, chills, sweats, fatigue, and malaise. These symptoms are often more pronounced in bacterial pneumonia.
- Vital Signs: Vital signs may show an elevated respiratory rate (tachypnea), increased heart rate (tachycardia), and fever. In severe cases, hypotension and altered mental status can occur.
- Physical Examination Findings: On physical examination, findings may include crackles or wheezing on lung auscultation, dullness to percussion over the affected area, and sometimes bronchial breath sounds if consolidation is present.
- Special Populations: In elderly patients or those with underlying chronic conditions, pneumonia may present atypically with confusion, worsening of underlying conditions, or without classic respiratory symptoms.
Diagnostic Dilemmas:
- Clinical Diagnosis vs. Radiographic Confirmation: It is often diagnosed clinically based on symptoms and physical examination findings, radiographic confirmation with chest X-ray or CT scan is usually required, especially in cases with atypical presentations or when complications are suspected.
- Distinguishing Bacterial vs. Viral Etiology: It can be challenging to differentiate between bacterial and viral pneumonia based solely on clinical presentation. Laboratory tests like sputum culture, blood cultures, and molecular assays can help identify the causative pathogen, but results may not be immediately available.
- Identifying Underlying Causes: It can be caused by a variety of pathogens, including bacteria, viruses, fungi, and parasites. Identifying the underlying cause is crucial for selecting appropriate antimicrobial therapy and preventing recurrence.
- Differentiating Community-Acquired vs. Hospital-Acquired Pneumonia: Distinguishing between community-acquired pneumonia (CAP) and hospital-acquired pneumonia (HAP) is essential for guiding initial empiric antibiotic therapy. However, the distinction can be challenging in patients with recent healthcare exposure or multiple comorbidities.
- Assessing Severity: Assessing the severity of pneumonia is crucial for determining the appropriate level of care and management strategy. Various scoring systems, such as the CURB-65 score or the Pneumonia Severity Index (PSI), can help stratify patients based on their risk of mortality and guide treatment decisions.
- Detecting Complications: It can lead to complications such as pleural effusion, empyema, lung abscess, septicemia, or acute respiratory distress syndrome (ARDS). Early recognition of these complications is vital for prompt intervention and improved outcomes.
Navigating these diagnostic dilemmas requires a comprehensive approach, including a detailed clinical evaluation, appropriate laboratory and imaging studies, and consideration of individual patient factors and risk factors. Collaboration between clinicians, radiologists, and infectious disease specialists is often necessary to optimize the management of patients with pneumonia.
Navigating the Therapeutic Landscape of Pneumonia: Treatment and Management Strategies
Navigating the therapeutic landscape it requires a multidimensional approach that addresses the underlying infection, mitigates inflammatory cascades, and supports vital organ function. This section will delve into the intricacies of pneumonia management, encompassing pharmacological interventions, supportive care measures, and adjunctive therapies aimed at optimizing patient outcomes.
Antimicrobial therapy forms the cornerstone treatment, with empirical antibiotic regimens tailored to the suspected microbial etiology and disease severity. However, the era of indiscriminate antibiotic use has ushered in a new era of antimicrobial stewardship, emphasizing the judicious use of antibiotics to mitigate the emergence of drug-resistant pathogens and minimize collateral damage to the host microbiome.
In addition to antimicrobial therapy, supportive measures such as oxygen supplementation, fluid resuscitation, and mechanical ventilation may be necessary in critically ill patients with severe pneumonia. Non-pharmacological interventions, including chest physiotherapy, early mobilization, and nutritional support, play pivotal roles in promoting recovery and mitigating the risk of complications.
Fortifying the Bastions: Prevention Strategies and Public Health Interventions
Fortifying the bastions against necessitates a concerted effort to bolster preventive strategies and public health interventions. This section will delve into the arsenal of preventive measures aimed at curbing the spread of pneumonia, including vaccination campaigns, infection control practices, and environmental interventions.
Vaccination stands as a formidable weapon in the fight against pneumonia, with vaccines targeting common pathogens such as Streptococcus pneumoniae, Haemophilus influenzae, and influenza virus. By immunizing vulnerable populations, including children, older adults, and individuals with chronic medical conditions, vaccination campaigns can effectively reduce the incidence of pneumonia and avert its associated morbidity and mortality.
In addition to vaccination, infection control practices such as hand hygiene, respiratory etiquette, and environmental sanitation play pivotal roles in preventing the spread of pneumonia in healthcare settings and communities. Public health interventions aimed at addressing socioeconomic disparities, improving access to healthcare, and mitigating environmental risk factors can further attenuate the burden of pneumonia and promote health equity.
Charting the Course Ahead: Research Frontiers and Future Directions
Charting the course ahead in research entails navigating uncharted waters, probing the frontiers of scientific inquiry, and harnessing innovative technologies to unravel the mysteries of this enigmatic disease. This section will illuminate the research frontiers and future directions in pneumonia research, delineating the challenges, opportunities, and paradigm shifts that lie on the horizon.
Emerging trends in pneumonia research encompass a diverse array of disciplines, ranging from molecular microbiology and immunology to epidemiology and health systems research. Advances in diagnostic technologies, such as next-generation sequencing and point-of-care testing, hold promise for enhancing pneumonia diagnosis and identifying novel therapeutic targets.
Future directions in research encompass a multifaceted approach that integrates basic science discoveries with translational research and implementation science. By fostering interdisciplinary collaborations, leveraging big data analytics, and embracing innovative methodologies, researchers can accelerate progress towards preventing, diagnosing, and treating pneumonia more effectively.
Conclusion: Illuminating the Path Forward
In conclusion, it is imperative to acknowledge that pneumonia’s enduring presence in global health necessitates a concerted and sustained effort to combat this insidious threat. As we reflect on the complexities of pneumonia and its far-reaching impact, it becomes evident that addressing this formidable foe requires a multifaceted approach that extends beyond traditional healthcare settings.
By fostering collaboration among stakeholders from diverse disciplines, including healthcare providers, researchers, policymakers, and community leaders, we can synergize efforts to enhance pneumonia prevention, diagnosis, and treatment. Multidisciplinary research endeavors aimed at elucidating the underlying mechanisms of pneumonia pathogenesis, identifying novel therapeutic targets, and developing innovative diagnostic tools hold promise for transforming the landscape of pneumonia management.
Moreover, investing in public health infrastructure, strengthening healthcare systems, and improving access to essential resources such as vaccines, antibiotics, and supportive care services are crucial steps towards mitigating the burden of pneumonia, particularly in resource-limited settings. By prioritizing equity, inclusivity, and sustainability in our interventions, we can ensure that all individuals, regardless of geographic location or socioeconomic status, have access to the care and resources needed to combat pneumonia effectively.
Furthermore, raising awareness about pneumonia’s impact on individual health, community well-being, and global prosperity is essential for galvanizing support and mobilizing resources towards this critical cause. Education campaigns, advocacy initiatives, and community engagement efforts can empower individuals to take proactive measures to prevent pneumonia, recognize early signs and symptoms, and seek timely medical attention when needed.
In addition to conventional approaches, harnessing the power of technology, innovation, and digital health solutions holds immense potential for revolutionizing pneumonia care delivery and enhancing health outcomes. Telemedicine platforms, remote monitoring devices, and mobile health applications can facilitate timely access to healthcare services, enable real-time monitoring of disease progression, and empower patients to actively participate in their care.
Ultimately, the fight against pneumonia requires a collective commitment to prioritize health equity, foster innovation, and strengthen global partnerships. By embracing a collaborative, multidisciplinary approach and leveraging the collective expertise and resources of the global community, we can overcome the challenges posed by pneumonia and usher in a future where every individual can breathe freely, unencumbered by the specter of this silent killer. Together, we can turn the tide against pneumonia and pave the way for a healthier, more resilient world for generations to come. For More More Information you can check our blogs “Drugs: Navigating the Pharmacological Perils and Dynamic Interplay with Disease”.
