Great Health Great Fitness
“Women’s Backbone Wellness: Insights into Spinal Disc Challenges – Risks, Symptoms, and Treatment Strategies”
Explore effective coping strategies and treatment options for spinal disc issues with our comprehensive guide. From understanding symptoms to implementing treatment strategies, empower yourself to manage spinal disc issues and improve your quality of life.
Introduction
Women’s Backbone Wellness: Insights into Spinal Disc Challenges Women’s Backbone Wellness: Insights into Spinal Disc ChallengesWomen’s Backbone Wellness: Insights into Spinal Disc Challenges Women’s Backbone Wellness: Insights into Spinal Disc ChallengesWomen’s Backbone Wellness: Insights into Spinal Disc Challenges Women’s Backbone Wellness: Insights into Spinal Disc ChallengesWomen’s Backbone Wellness: Insights into Spinal Disc Challenges Women’s Backbone Wellness: Insights into Spinal Disc ChallengesWomen’s Backbone Wellness: Insights into Spinal Disc Challenges Women’s Backbone Wellness: Insights into Spinal Disc ChallengesWomen’s Backbone Wellness: Insights into Spinal Disc Challenges Women’s Backbone Wellness: Insights into Spinal Disc Challenges
Understanding Spinal Discs
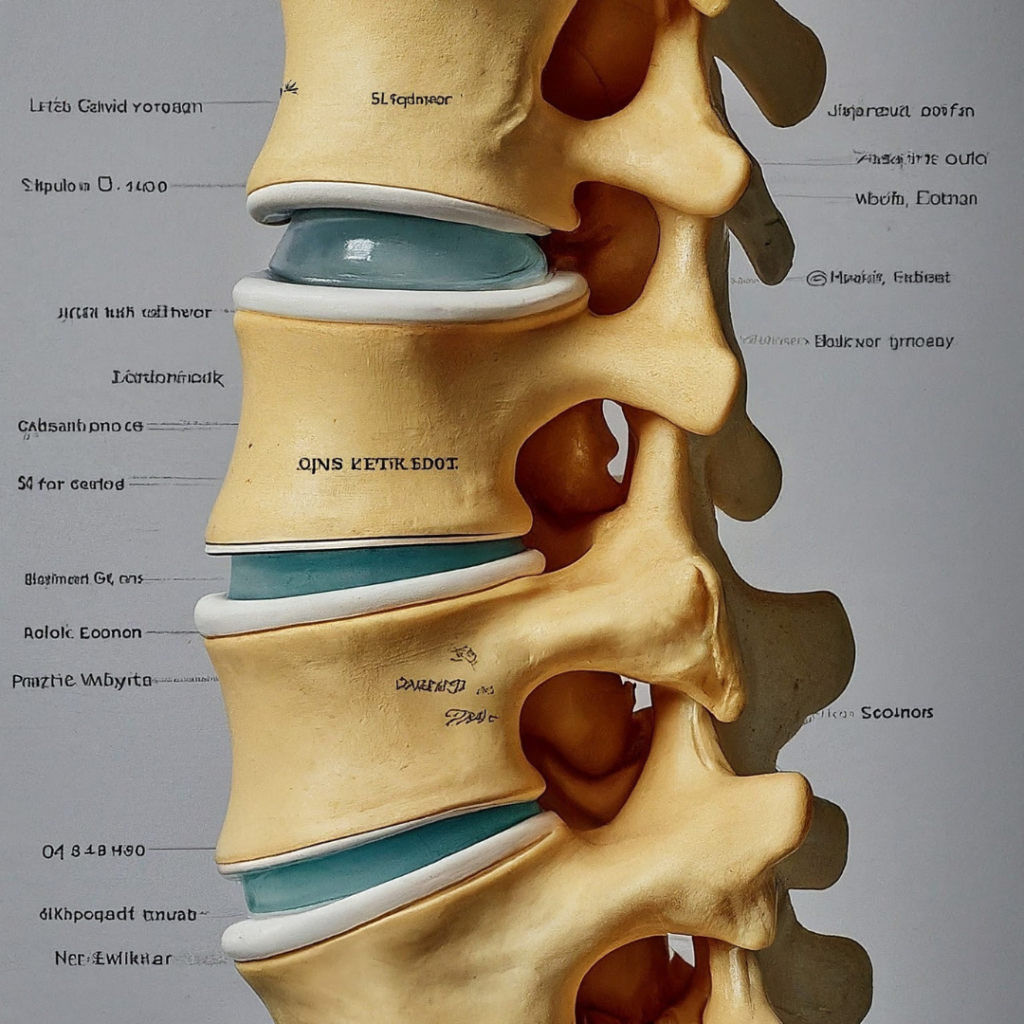
The spine is a crucial component of the human body, providing structural support, flexibility, and protection for the spinal cord. Central to its function are the intervertebral discs, which act as shock absorbers between the vertebrae. Each disc consists of a tough outer layer (annulus fibrosus) and a gel-like inner core (nucleus pulposus). The composition of spinal discs allows for movement while maintaining stability, making them essential for everyday activities such as walking, bending, and twisting.
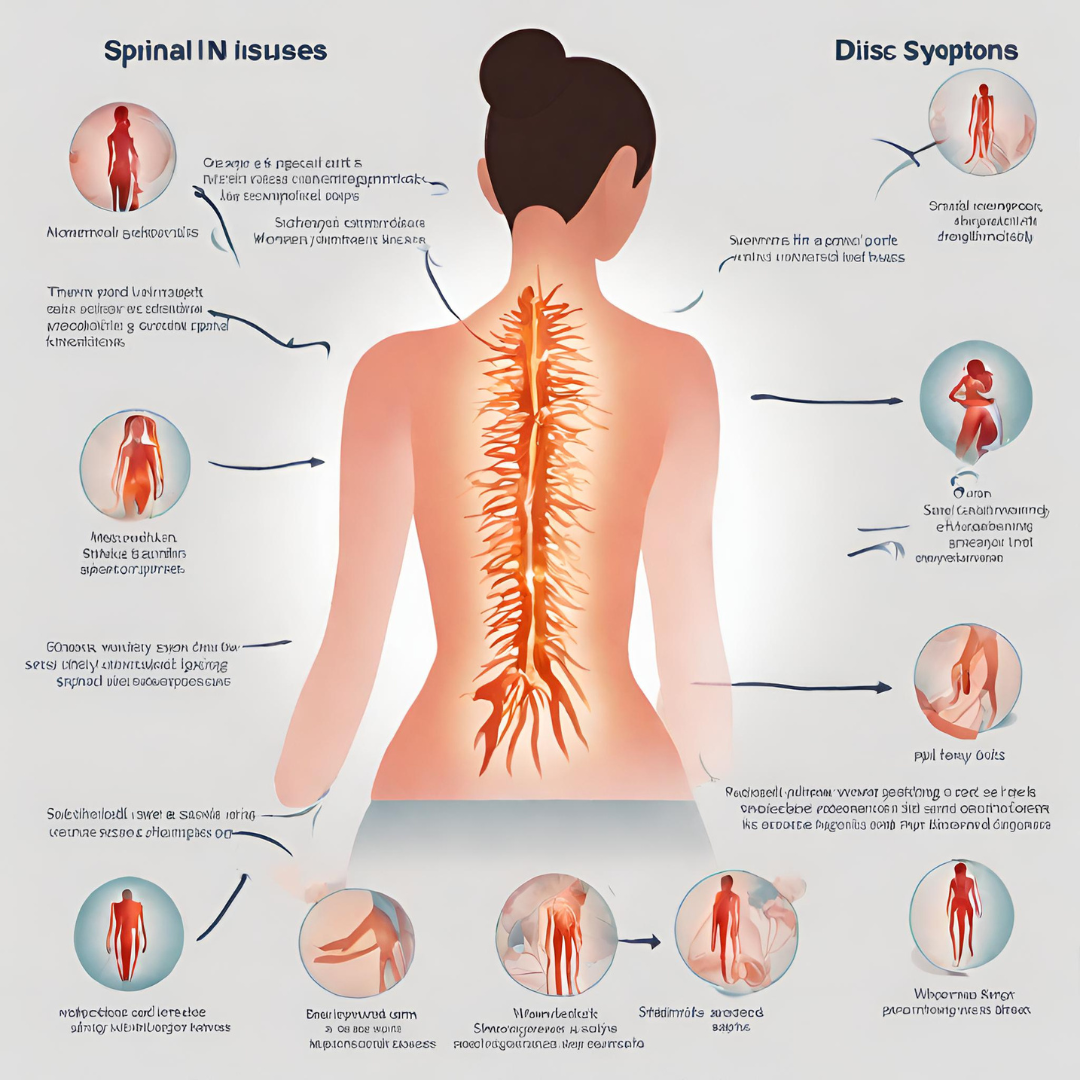
Common Spinal Disc Issues in Women
- Degenerative Disc Disease (DDD) Degenerative disc disease is a condition characterized by the gradual breakdown of spinal discs over time. While aging is a primary risk factor for DDD, other factors such as genetics, lifestyle choices, and injuries can contribute to its development. As women age, hormonal changes associated with menopause may also influence the degenerative process. Symptoms of DDD may include chronic low back pain, stiffness, and reduced mobility. Diagnosis often involves a combination of physical examination, imaging studies (e.g., MRI), and diagnostic injections to confirm the source of pain.
- Herniated Discs Also known as a slipped or ruptured disc, a herniated disc occurs when the soft inner core of a spinal disc protrudes through the tough outer layer, often due to trauma or repetitive stress. Women are susceptible to herniated discs during pregnancy and childbirth due to the increased strain on the spine and pelvic region. Symptoms may vary depending on the location and severity of the herniation but commonly include localized or radiating pain, numbness, tingling, and muscle weakness. Treatment options range from conservative measures such as rest, physical therapy, and medications to more invasive interventions like epidural steroid injections or surgery.
- Disc Bulge A disc bulge refers to a protrusion of the disc’s outer layer beyond its normal boundaries, typically caused by wear and tear or injury. While similar to a herniated disc, a disc bulge may not involve the rupture of the inner core. Women may experience disc bulges as a result of repetitive movements, poor posture, or degenerative changes associated with aging. Symptoms can vary widely but often include localized back pain, stiffness, and discomfort with certain movements. Treatment typically involves a combination of conservative measures, including physical therapy, pain management, and lifestyle modifications.
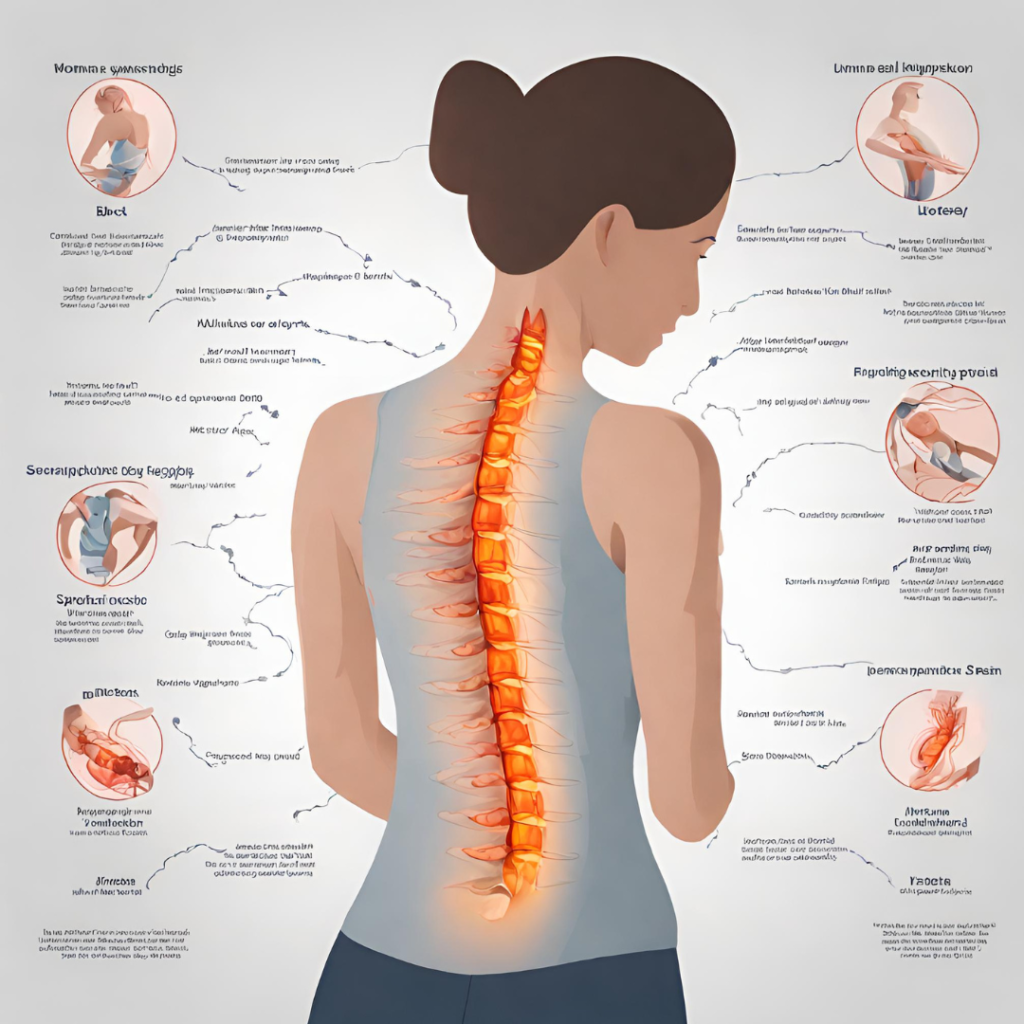
Risk Factors for Spinal Disc Issues in Women
Several factors contribute to the development of spinal disc issues in women:
- Age-related Changes: As women age, the intervertebral discs undergo natural degenerative changes, such as loss of hydration and elasticity, which can increase the risk of disc-related problems.
- Hormonal Influences: Hormonal fluctuations during puberty, pregnancy, and menopause can affect the integrity of spinal discs and may contribute to the development or exacerbation of disc issues.
- Pregnancy and Childbirth: The physical demands of pregnancy, including weight gain and changes in posture, place increased strain on the spine and pelvic region, potentially leading to disc herniation or other related conditions.
- Lifestyle Factors: Sedentary lifestyle, poor posture, and obesity can all contribute to the development of spinal disc issues by placing excessive stress on the spine and increasing the risk of degenerative changes.
- Occupational Hazards: Jobs that involve heavy lifting, repetitive movements, or prolonged sitting can increase the risk of disc-related problems, particularly if proper ergonomic precautions are not observed.
Symptoms of Spinal Disc Issues in Women
Spinal disc issues can cause a range of symptoms, which may vary depending on the type and severity of the condition:
- Back Pain: Chronic or intermittent pain in the lower back, upper back, or neck is a common symptom of spinal disc issues. The pain may be dull, achy, or sharp and may worsen with movement or certain activities.
- Radiating Pain: Discomfort that radiates from the site of the affected disc to other areas of the body, such as the buttocks, legs, arms, or shoulders, is often indicative of nerve compression or irritation.
- Numbness and Tingling: Sensations of numbness, tingling, or pins-and-needles in the extremities may occur when a spinal disc impinges on nearby nerves, disrupting normal sensory signals.
- Muscle Weakness: Weakness or decreased muscle strength in the affected area may result from nerve compression or impaired nerve function caused by spinal disc issues.
- Changes in Bowel or Bladder Function: In severe cases of spinal cord compression, individuals may experience changes in bowel or bladder function, such as urinary incontinence or difficulty controlling bowel movements.
It is essential for women to be aware of these symptoms and seek prompt medical evaluation if they experience persistent or worsening back pain or related symptoms.
Diagnosis of Spinal Disc Issues in Women
Diagnosing spinal disc issues in women typically involves a comprehensive evaluation, including:
- Medical History: A detailed history of symptoms, past medical conditions, and relevant lifestyle factors can provide valuable insights into the underlying cause of spinal disc issues.
- Physical Examination: A physical examination allows healthcare providers to assess posture, range of motion, muscle strength, and neurological function, which can help localize the source of symptoms.
- Imaging Studies: Imaging tests such as X-rays, magnetic resonance imaging (MRI), or computed tomography (CT) scans may be ordered to visualize the spinal structures and identify any abnormalities, such as disc herniation, degenerative changes, or spinal stenosis.
- Diagnostic Injections: In some cases, diagnostic injections such as epidural steroid injections or nerve blocks may be used to confirm the source of pain and assess the effectiveness of targeted treatments.
Once a diagnosis is established, healthcare providers can develop an individualized treatment plan tailored to the woman’s specific needs and preferences.
Treatment Strategies for Spinal Disc Issues
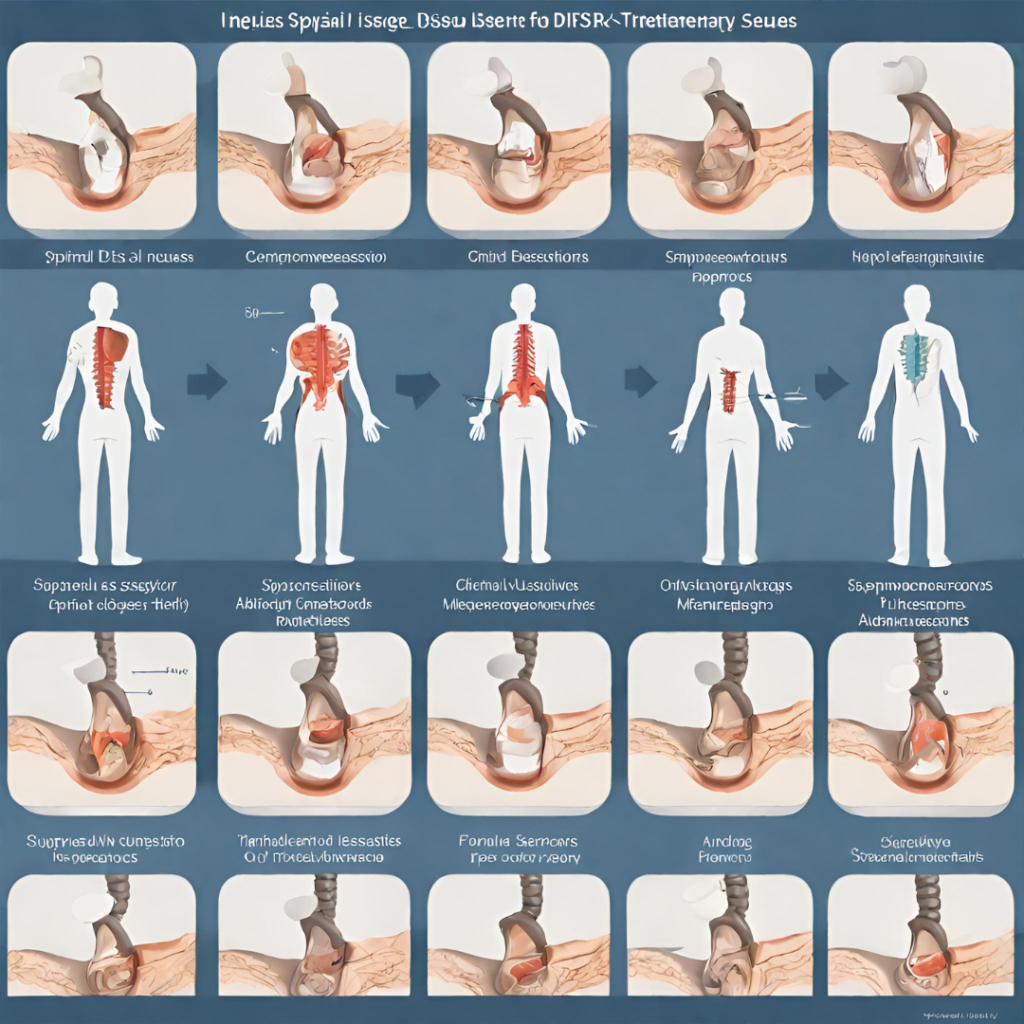
The management of spinal disc issues in women typically involves a combination of conservative measures, interventional treatments, and surgical interventions:
- Conservative Management: Conservative approaches aim to alleviate symptoms, improve function, and promote long-term spinal health through non-invasive or minimally invasive methods. Common conservative treatments for spinal disc issues may include:
- Rest and Activity Modification: Temporary rest combined with gradual return to light activity can help reduce pain and inflammation and prevent further aggravation of symptoms.
- Physical Therapy: Targeted exercises, stretches, and manual therapy techniques can help strengthen the muscles surrounding the spine, improve flexibility, and correct postural imbalances.
- Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), muscle relaxants, and analgesics may be prescribed to alleviate pain and inflammation associated with spinal disc issues.
- Heat and Cold Therapy: Application of heat packs or cold packs to the affected area can help relieve muscle tension, reduce pain, and promote relaxation.
- Bracing: External supports such as lumbar braces or corsets may provide temporary stability and pain relief for individuals with spinal disc issues.
- Education and Self-care: Patient education on proper body mechanics, ergonomic principles, and self-management strategies can empower women to take an active role in managing their spinal health.
- Interventional Treatments: When conservative measures fail to provide adequate relief, or in cases of severe or persistent symptoms, interventional treatments may be considered to target the source of pain more directly. Common interventional treatments for spinal disc issues may include:
- Epidural Steroid Injections: Corticosteroid medications injected into the epidural space surrounding the spinal cord and nerve roots can help reduce inflammation and alleviate pain associated with spinal disc issues.
- Facet Joint Injections: Injection of local anesthetics and corticosteroids into the facet joints of the spine can provide temporary pain relief and diagnostic information in cases of suspected facet joint dysfunction.
- Nerve Blocks: Selective nerve blocks involve the injection of local anesthetic medications near specific nerves to block pain signals and provide temporary relief from symptoms.
- Radiofrequency Ablation: Radiofrequency ablation (RFA) uses heat generated by radiofrequency waves to disrupt nerve conduction and reduce pain signals from the affected nerves.
- Surgical Options: In cases where conservative and interventional treatments fail to provide sufficient relief, or when spinal disc issues cause significant neurological deficits or impairment of daily function, surgical intervention may be considered. Common surgical procedures for spinal disc issues may include:
- Discectomy: A discectomy involves the removal of a portion of the affected disc to relieve pressure on nearby nerves and alleviate symptoms of nerve compression.
- Microdiscectomy: Microdiscectomy is a minimally invasive surgical technique that uses specialized instruments and magnification to remove herniated disc material while preserving surrounding structures.
- Spinal Fusion: Spinal fusion surgery involves joining two or more vertebrae together using bone grafts, screws, or metal rods to stabilize the spine and promote fusion of the affected segments.
- Artificial Disc Replacement: In cases of disc degeneration or herniation, artificial disc replacement may be considered as an alternative to traditional fusion surgery, preserving motion and flexibility in the spine.
- Complementary and Alternative Therapies: In addition to conventional medical treatments, some women may benefit from complementary and alternative therapies to manage symptoms and improve overall well-being. Examples of complementary and alternative therapies for spinal disc issues may include:
- Acupuncture: Acupuncture involves the insertion of thin needles into specific points on the body to stimulate nerve pathways and promote pain relief, relaxation, and healing.
- Chiropractic Care: Chiropractic adjustments and spinal manipulation techniques aim to restore proper alignment and function of the spine, relieving pressure on affected discs and nerves.
- Yoga and Pilates: Yoga and Pilates exercises focus on strengthening the core muscles, improving posture, and enhancing flexibility, which can help alleviate symptoms and prevent future episodes of spinal disc issues.
- Mind-body Techniques: Mindfulness meditation, guided imagery, and relaxation techniques can help reduce stress, alleviate muscle tension, and improve coping skills for managing chronic pain associated with spinal disc issues.
The choice of treatment approach will depend on various factors, including the woman’s overall health, the severity of symptoms, the underlying cause of spinal disc issues, and her personal preferences. A multidisciplinary approach involving collaboration between healthcare providers, physical therapists, pain specialists, and other allied health professionals may be beneficial in optimizing outcomes and improving quality of life for women with spinal disc issues.
Prevention and Lifestyle Modifications
While some risk factors for spinal disc issues, such as age and genetics, cannot be modified, women can take proactive steps to maintain spinal health and reduce the risk of developing disc-related problems:
- Maintain a Healthy Weight: Excess body weight can place added stress on the spine and increase the risk of disc degeneration and herniation. Adopting a balanced diet and engaging in regular physical activity can help achieve and maintain a healthy weight.
- Regular Exercise and Physical Activity: Participating in regular exercise programs that include strength training, cardiovascular exercise, and flexibility exercises can help strengthen the muscles supporting the spine, improve posture, and reduce the risk of spinal disc issues.
- Proper Posture and Body Mechanics: Practicing good posture and body mechanics during daily activities, such as sitting, standing, lifting, and bending, can help distribute forces evenly across the spine and reduce the risk of strain or injury to spinal discs.
- Ergonomic Considerations in the Workplace: Ergonomic modifications to workstations and equipment can help minimize the risk of repetitive strain injuries and promote proper spinal alignment. Adjustments such as ergonomic chairs, standing desks, and frequent breaks can help reduce the risk of spinal disc issues among women who work sedentary jobs.
- Smoking Cessation: Smoking has been linked to accelerated disc degeneration and impaired healing processes, increasing the risk of spinal disc issues. Quitting smoking can improve circulation, reduce inflammation, and promote tissue repair, leading to better spinal health.
- Strategies for Managing Stress: Chronic stress can contribute to muscle tension, pain sensitivity, and poor coping mechanisms, exacerbating symptoms of spinal disc issues. Incorporating stress management techniques such as relaxation exercises, mindfulness meditation, and deep breathing can help alleviate stress and promote relaxation, supporting overall spinal health.
By adopting these preventive measures and lifestyle modifications, women can take an active role in preserving spinal health and reducing the risk of developing spinal disc issues over time.
Living with Spinal Disc Issues: Coping Strategies

Living with spinal disc issues can present physical, emotional, and practical challenges for women. However, with the right support and coping strategies, individuals can manage their symptoms effectively and maintain a good quality of life:
- Education and Self-management Techniques: Learning about the nature of spinal disc issues, their underlying causes, and available treatment options can empower women to make informed decisions about their care. Healthcare providers can provide guidance on self-management techniques, such as proper body mechanics, ergonomic principles, and activity modifications, to help minimize symptoms and prevent exacerbations.
- Supportive Resources: Support groups, online forums, and community organizations can provide valuable emotional support, practical advice, and shared experiences for women living with spinal disc issues. Connecting with others who are facing similar challenges can reduce feelings of isolation and provide a sense of belonging and understanding.
- Psychological Support: Chronic pain and disability associated with spinal disc issues can take a toll on mental health and well-being. Seeking support from mental health professionals, such as therapists or counselors, can help women develop coping skills, manage stress, and address emotional concerns related to their condition.
- Adaptive Devices and Assistive Technology: Assistive devices and adaptive aids, such as ergonomic chairs, lumbar cushions, or mobility aids, can help women with spinal disc issues perform daily activities more comfortably and independently. Healthcare providers can recommend appropriate assistive devices based on individual needs and functional limitations.
By incorporating these coping strategies into their daily lives, women can effectively manage the physical and emotional challenges associated with spinal disc issues and maintain a positive outlook on their health and well-being.
Conclusion
In conclusion, spinal disc issues can significantly impact women’s spinal health, mobility, and quality of life. Understanding the risk factors, symptoms, diagnosis, and treatment options for spinal disc issues is essential for effective management and prevention. By adopting preventive measures, lifestyle modifications, and coping strategies, women can take proactive steps to preserve spinal health, reduce the risk of developing disc-related problems, and optimize their overall well-being. For More Information you can check our blogs “Unraveling the Mystery of Back Pain: 9 common Causes, Symptoms, and Management Strategies”.
