I. Introduction to Neurological Disorders
Neurological disorders encompass a broad spectrum of conditions affecting the nervous system, including the brain, spinal cord, and peripheral nerves. These disorders can arise from various causes, including genetic factors, environmental influences, infections, trauma, and autoimmune reactions. Understanding neurological disorders is crucial due to their significant impact on individuals’ quality of life, as well as their socioeconomic burden on society.
Neurological disorders can manifest with diverse symptoms, ranging from cognitive impairment and motor dysfunction to sensory disturbances and autonomic dysfunction. They may present with acute, episodic, or chronic symptoms, often requiring multidisciplinary approaches for diagnosis, management, and rehabilitation.
The prevalence of neurological disorders varies across populations and age groups, with some conditions being more prevalent in certain demographics or geographical regions. Additionally, advancements in medical technology and diagnostic techniques have led to improved detection and management of neurological conditions, although challenges remain in addressing treatment gaps and ensuring equitable access to care.
II. Anatomy and Function of the Nervous System
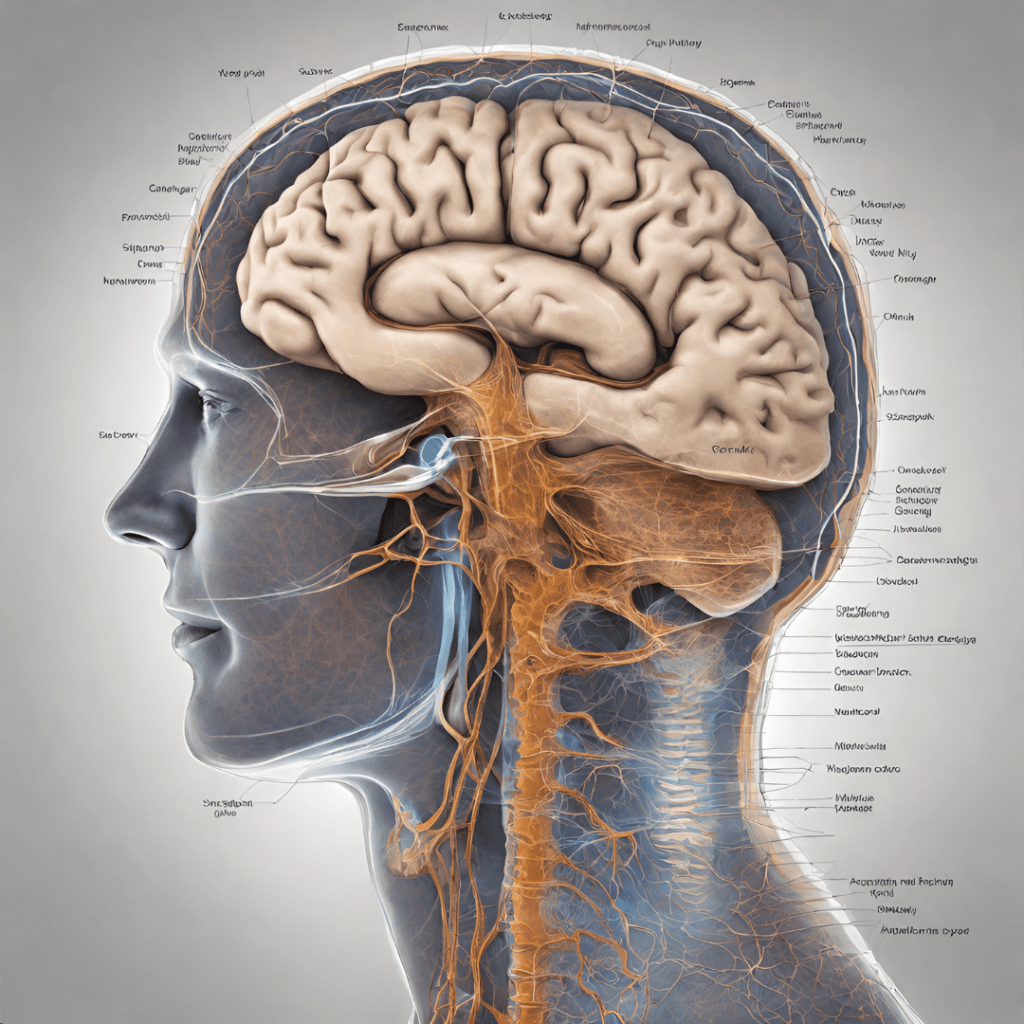
The nervous system comprises the central nervous system (CNS), consisting of the brain and spinal cord, and the peripheral nervous system (PNS), comprising the nerves that connect the CNS to the rest of the body. Neurons are the basic building blocks of the nervous system, transmitting electrochemical signals to facilitate communication between different parts of the body.
The CNS plays a central role in regulating bodily functions, including sensory perception, motor control, cognition, and emotional responses. The PNS extends from the CNS to innervate organs, muscles, and glands, coordinating voluntary and involuntary actions.
Neurotransmitters are chemical messengers that facilitate communication between neurons, enabling the transmission of signals across synapses. Imbalances in neurotransmitter levels or receptor function can contribute to the pathogenesis of neurological disorders, underscoring the importance of neurotransmitter modulation in treatment strategies.
Understanding the anatomy and function of the nervous system is essential for elucidating the pathophysiology of neurological disorders and developing targeted interventions to restore normal function and alleviate symptoms.
III. Classification of Neurological Disorders
Neurological disorders encompass a diverse array of conditions, classified based on various criteria, including etiology, affected anatomical structures, and clinical manifestations. Broadly, neurological disorders can be categorized into primary neurodegenerative disorders, neurodevelopmental disorders, neuroinflammatory disorders, and neurological trauma.
Primary neurodegenerative disorders involve progressive degeneration of neurons or their supporting structures, leading to cognitive decline, movement disorders, or sensory deficits. Examples include Alzheimer’s disease, Parkinson’s disease, and amyotrophic lateral sclerosis (ALS).
Neurodevelopmental disorders manifest during early childhood and are characterized by abnormalities in brain development, resulting in deficits in social interaction, communication, and behavior. Autism spectrum disorder (ASD), attention deficit hyperactivity disorder (ADHD), and intellectual disability are examples of neurodevelopmental disorders.
Neuroinflammatory disorders involve inflammation of the nervous system, often triggered by autoimmune reactions, infections, or environmental factors. Multiple sclerosis (MS), Guillain-Barré syndrome, and encephalitis are examples of neuroinflammatory disorders.
Neurological trauma encompasses injuries to the nervous system resulting from physical trauma, such as traumatic brain injury (TBI), spinal cord injury (SCI), and peripheral nerve injuries.
Understanding the classification of neurological disorders facilitates accurate diagnosis, treatment selection, and prognostic assessment, guiding clinical management and research efforts.
IV. Common Neurological Disorders
Epilepsy Epilepsy is a chronic neurological disorder characterized by recurrent seizures, which are sudden, uncontrolled electrical disturbances in the brain. Seizures can manifest with various symptoms, including convulsions, loss of consciousness, sensory disturbances, or altered behavior. The underlying mechanisms of epilepsy involve abnormal neuronal excitability and synchronization, leading to hypersynchronous electrical activity in the brain.
Stroke Stroke, also known as cerebrovascular accident (CVA), occurs when blood flow to a part of the brain is disrupted, resulting in ischemia (ischemic stroke) or hemorrhage (hemorrhagic stroke). Ischemic strokes are more common and typically result from thrombotic or embolic occlusion of cerebral arteries, depriving brain tissue of oxygen and nutrients. Hemorrhagic strokes occur due to rupture of blood vessels within the brain, leading to bleeding and subsequent damage to surrounding tissue.
Alzheimer’s Disease Alzheimer’s disease is a progressive neurodegenerative disorder characterized by cognitive decline, memory impairment, and behavioral changes. Pathologically, Alzheimer’s disease is characterized by the accumulation of abnormal protein aggregates, including beta-amyloid plaques and tau tangles, in the brain. These pathological changes lead to synaptic dysfunction, neuronal loss, and brain atrophy, resulting in the characteristic clinical manifestations of the disease.
Parkinson’s Disease Parkinson’s disease is a chronic neurodegenerative disorder characterized by motor symptoms such as tremors, bradykinesia (slowed movement), rigidity, and postural instability. The primary pathology of Parkinson’s disease involves the degeneration of dopaminergic neurons in the substantia nigra region of the brain, leading to dopamine deficiency and disruption of basal ganglia circuitry. In addition to motor symptoms, Parkinson’s disease may also manifest with non-motor symptoms, including cognitive impairment, autonomic dysfunction, and psychiatric disturbances.
V. Less Common Neurological Disorders
Multiple Sclerosis (MS) Multiple sclerosis is an autoimmune inflammatory demyelinating disorder of the central nervous system (CNS), characterized by recurrent episodes of neurological dysfunction due to inflammation, demyelination, and axonal injury. The underlying cause of MS is thought to involve dysregulated immune responses targeting myelin, the protective sheath surrounding nerve fibers in the CNS. MS can manifest with a wide range of symptoms, including sensory disturbances, motor weakness, visual impairment, and cognitive dysfunction.
Amyotrophic Lateral Sclerosis (ALS) Amyotrophic lateral sclerosis, also known as Lou Gehrig’s disease, is a progressive neurodegenerative disorder characterized by the degeneration of motor neurons in the brain and spinal cord, leading to muscle weakness, atrophy, and eventual paralysis. The exact cause of ALS remains unclear, although genetic mutations, environmental factors, and aberrant protein aggregation have been implicated in disease pathogenesis. ALS typically presents with progressive muscle weakness and wasting, eventually affecting respiratory function and leading to death within a few years of diagnosis.
Huntington’s Disease Huntington’s disease is an inherited neurodegenerative disorder caused by a mutation in the HTT gene, leading to the production of abnormal huntingtin protein aggregates that accumulate in the brain. Huntington’s disease is characterized by progressive motor dysfunction, cognitive decline, and psychiatric disturbances. Symptoms typically manifest in mid-adulthood and worsen over time, ultimately leading to severe disability and premature death. Currently, there is no cure for Huntington’s disease, and treatment focuses on managing symptoms and improving quality of life.
VI. Pediatric Neurological Disorders
Cerebral Palsy Cerebral palsy is a group of non-progressive neurological disorders that affect movement, posture, and muscle coordination, resulting from abnormal brain development or injury during early childhood. The etiology of cerebral palsy can vary, including prenatal factors such as intrauterine infections or maternal health conditions, perinatal factors such as birth trauma or asphyxia, and postnatal factors such as infections or head injuries. Cerebral palsy is characterized by motor impairments, which can range from mild to severe and may be accompanied by associated conditions such as intellectual disability, epilepsy, or sensory impairments.
Autism Spectrum Disorder (ASD) Autism spectrum disorder is a neurodevelopmental disorder characterized by persistent deficits in social communication and interaction, as well as restricted, repetitive patterns of behavior, interests, or activities. The exact cause of ASD remains unknown, although both genetic and environmental factors are believed to play a role in its etiology. ASD is typically diagnosed in early childhood, with symptoms varying in severity and presentation across individuals. Early intervention and behavioral therapies can help improve outcomes for individuals with ASD, although challenges may persist throughout the lifespan.
VII. Diagnosis and Evaluation of Neurological Disorders
Diagnosing neurological disorders requires a comprehensive evaluation that may include clinical history, physical examination, neuroimaging studies, electrophysiological tests, and laboratory investigations.
Clinical History: Gathering a detailed history of the patient’s symptoms, medical history, family history, and environmental exposures is essential for identifying potential risk factors and guiding further evaluation.
Physical Examination: A thorough neurological examination assesses various aspects of neurological function, including cranial nerve function, motor strength, sensation, coordination, reflexes, and gait. Abnormal findings on examination may provide clues to the underlying neurological disorder.
Neuroimaging Studies: Imaging modalities such as magnetic resonance imaging (MRI), computed tomography (CT), and positron emission tomography (PET) can provide detailed anatomical and functional information about the brain and spinal cord. These studies are valuable for identifying structural abnormalities, lesions, or other pathological changes associated with neurological disorders.
Electrophysiological Tests: Electrophysiological studies such as electroencephalography (EEG), electromyography (EMG), and nerve conduction studies (NCS) assess the electrical activity of the brain, muscles, and peripheral nerves, respectively. These tests can help diagnose conditions such as epilepsy, neuropathy, and neuromuscular disorders.
Laboratory Investigations: Blood tests, cerebrospinal fluid analysis, and genetic testing may be performed to evaluate biochemical, immunological, or genetic factors associated with neurological disorders. These tests can help confirm diagnoses, identify underlying causes, or assess treatment response.
Multimodal Approach: Combining multiple diagnostic modalities allows for a comprehensive assessment of neurological function and pathology, facilitating accurate diagnosis and treatment planning. Collaboration among neurologists, neurosurgeons, radiologists, and other healthcare professionals is essential for optimizing diagnostic strategies and patient care.
VIII. Treatment Approaches for Neurological Disorders
Treatment of neurological disorders aims to alleviate symptoms, slow disease progression, and improve patients’ quality of life. Therapeutic interventions may include pharmacotherapy, surgical procedures, rehabilitation therapies, and lifestyle modifications.
Pharmacotherapy: Medications play a central role in managing neurological disorders by modulating neurotransmitter function, reducing inflammation, or targeting specific pathological mechanisms. Commonly prescribed medications include antiepileptic drugs, antiparkinsonian agents, immunomodulators, analgesics, and psychotropic medications.
Surgical Interventions: Surgical procedures may be indicated for certain neurological disorders refractory to medical management or associated with structural abnormalities requiring intervention. Examples include epilepsy surgery, deep brain stimulation (DBS) for movement disorders, tumor resection, and decompressive surgery for intracranial hypertension.
Rehabilitation Therapies: Physical therapy, occupational therapy, speech therapy, and cognitive rehabilitation are integral components of comprehensive care for neurological disorders. These therapies aim to improve functional abilities, mobility, communication skills, and cognitive function, enhancing patients’ independence and quality of life.
Complementary and Alternative Medicine (CAM): Some patients with neurological disorders may benefit from complementary and alternative therapies such as acupuncture, massage therapy, chiropractic manipulation, herbal supplements, or mind-body practices. While evidence supporting the efficacy of these interventions varies, they may provide adjunctive benefits or symptom relief for some individuals.
Multidisciplinary Care: Managing neurological disorders often requires a multidisciplinary approach involving neurologists, neurosurgeons, physiatrists, psychologists, rehabilitation specialists, and other healthcare professionals. Collaborative care teams work together to address patients’ complex needs, optimize treatment outcomes, and provide holistic support throughout the continuum of care.
Conclusion
Understanding neurological disorders is essential for healthcare professionals, patients, caregivers, and society as a whole. These conditions encompass a wide range of disorders affecting the nervous system, with diverse etiologies, clinical manifestations, and treatment approaches. Despite the complexity of neurological disorders, advances in medical research, diagnostic techniques, and therapeutic interventions have improved our ability to diagnose, treat, and manage these conditions.
Neurological disorders pose significant challenges to patients, caregivers, and healthcare systems, often resulting in substantial disability, reduced quality of life, and socioeconomic burden. Addressing the multifaceted needs of individuals with neurological disorders requires a comprehensive and multidisciplinary approach that integrates medical, psychological, social, and rehabilitative interventions.
Future advancements in neuroscience, genetics, pharmacology, and technology hold promise for further understanding the underlying mechanisms of neurological disorders and developing novel therapies to improve outcomes. However, addressing the complex challenges posed by neurological disorders will require continued investment in research, education, healthcare infrastructure, and public awareness initiatives.
By fostering collaboration among researchers, clinicians, policymakers, advocacy groups, and community stakeholders, we can work together to advance the field of neurology, enhance patient care, and ultimately improve the lives of individuals affected by neurological disorders.
In conclusion, while neurological disorders present significant clinical and societal challenges, they also inspire hope for progress and innovation in the quest for better understanding, treatment, and ultimately, prevention of these conditions. Through concerted efforts and collective action, we can strive to alleviate the burden of neurological disorders and promote brain health and well-being for all. For More Information you can check our blogs “Navigating Stress in the Modern World: 7 Strategies for Better Mental Health”.