Great Health Great Fitness
Leukopenia: Unraveling Deficiency, Symptoms, and Effective Treatments
"Leukopenia presents a complex challenge, characterized by a deficiency in white blood cells crucial for the body's immune defense. Understanding its symptoms and diagnosis is paramount for timely intervention. Treatment strategies range from medications to lifestyle modifications, emphasizing the holistic approach necessary for effective management. By unraveling the intricacies of leukopenia and adopting appropriate interventions, individuals can optimize their health outcomes and quality of life."
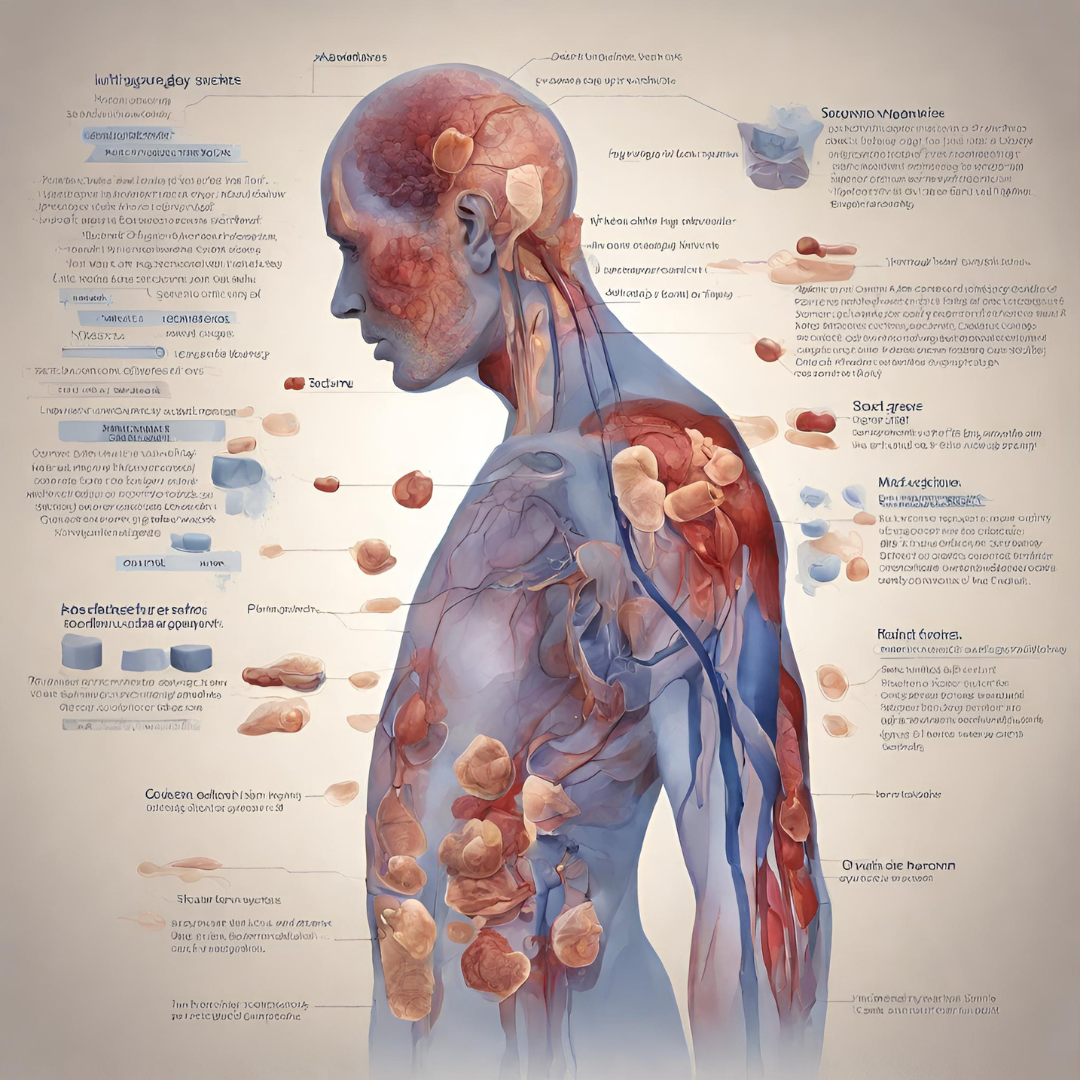
I. Introduction to Leukopenia
Leukopenia is a medical condition characterized by a decrease in the number of white blood cells (leukocytes) in the bloodstream, leading to an impaired immune response and increased susceptibility to infections. In this comprehensive guide, we will delve into the causes, symptoms, diagnosis, and treatment strategies for leukopenia, empowering individuals with knowledge and insights to manage this condition effectively.
Understanding Leukopenia: It is, also known as leukocytopenia, can result from various underlying factors that disrupt the production, distribution, or function of white blood cells. While a certain degree of fluctuation in white blood cell counts is normal, persistent or severe leukopenia can pose significant health risks and requires medical evaluation and intervention.
II. Causes of Leukopenia
1. Bone Marrow Disorders: Bone marrow disorders such as aplastic anemia, myelodysplastic syndromes (MDS), and leukemia can impair the production of white blood cells, leading to leukopenia. These conditions may arise from genetic mutations, exposure to toxins or radiation, or autoimmune reactions targeting the bone marrow.
2. Infections: Certain viral, bacterial, fungal, and parasitic infections can cause leukopenia by directly suppressing white blood cell production or inducing their destruction. Examples include HIV/AIDS, cytomegalovirus (CMV), Epstein-Barr virus (EBV), hepatitis, tuberculosis, malaria, and sepsis.
3. Medications and Treatments: Some medications, particularly chemotherapy drugs, immunosuppressants, and antibiotics, can cause leukopenia as a side effect. Radiation therapy, used in cancer treatment, can also suppress bone marrow function and reduce white blood cell counts.
4. Autoimmune Disorders: Autoimmune diseases such as lupus, rheumatoid arthritis, and autoimmune neutropenia can trigger immune reactions against white blood cells, leading to their destruction and subsequent leukopenia.
5. Nutritional Deficiencies: Deficiencies in certain nutrients, including vitamin B12, folate, copper, and zinc, can impair white blood cell production and contribute to leukopenia. Malnutrition, inadequate dietary intake, malabsorption disorders, and gastrointestinal surgeries can all impact nutrient absorption and utilization.
6. Congenital Disorders: Rare congenital disorders, such as Kostmann syndrome and cyclic neutropenia, are characterized by inherited abnormalities in white blood cell production or function, resulting in recurrent episodes of leukopenia and increased susceptibility to infections.
7. Environmental Factors: Exposure to environmental toxins, chemicals, heavy metals, and radiation can damage bone marrow cells and disrupt white blood cell production, leading to leukopenia. Occupational hazards and industrial pollutants may pose risks for individuals working in certain industries or environments.
III. Symptoms and Diagnosis of Leukopenia
Symptoms of Leukopenia: The symptoms of leukopenia can vary depending on the severity of the condition and the individual’s immune response. Common symptoms may include:
- Recurrent infections (such as respiratory infections, urinary tract infections, skin infections)
- Fever or chills
- Fatigue or weakness
- Easy bruising or bleeding
- Mouth ulcers or sore throat
- Swollen lymph nodes
- Persistent cough or shortness of breath
- Skin rashes or lesions
- Unexplained weight loss
Diagnostic Methods for Leukopenia:
- Complete Blood Count (CBC): A complete blood count is a standard laboratory test used to measure various components of the blood, including white blood cell count, red blood cell count, hemoglobin, hematocrit, and platelet count. A low white blood cell count (leukopenia) may indicate an underlying immune deficiency or bone marrow disorder.
- Peripheral Blood Smear: A peripheral blood smear involves examining a thin layer of blood under a microscope to evaluate the size, shape, and distribution of white blood cells. Abnormalities such as decreased numbers of white blood cells, immature white blood cells (blasts), or abnormal cell morphology may indicate underlying pathology.
- Bone Marrow Aspiration and Biopsy: In cases where leukopenia is suspected to arise from bone marrow disorders or malignancies, a bone marrow aspiration and biopsy may be performed to obtain a sample of bone marrow tissue for microscopic examination. This procedure can help assess cellularity, morphology, and the presence of abnormal cells or infiltrates.
- Infectious Disease Testing: If infectious causes of leukopenia are suspected, specific tests may be performed to identify viral, bacterial, fungal, or parasitic pathogens. Serological tests, molecular assays, cultures, and antigen/antibody detection methods may be used to diagnose infections and guide appropriate treatment.
- Autoimmune and Rheumatologic Testing: For individuals with suspected autoimmune causes of leukopenia, autoimmune antibody testing, inflammatory markers, and rheumatologic panels may be ordered to evaluate immune function and identify underlying autoimmune disorders.
IV. Treatment Strategies for Leukopenia

1. Addressing Underlying Causes: The treatment approach for leukopenia depends on identifying and addressing the underlying cause(s) of the condition. This may involve discontinuing medications that suppress white blood cell production, treating infections with appropriate antimicrobial agents, managing autoimmune disorders with immunosuppressive therapy, or addressing nutritional deficiencies through dietary modification or supplementation.
2. Medications to Stimulate White Blood Cell Production: In cases of severe leukopenia or bone marrow suppression, medications such as granulocyte colony-stimulating factor (G-CSF) or granulocyte-macrophage colony-stimulating factor (GM-CSF) may be prescribed to stimulate the production of white blood cells. These growth factors can help boost the immune response and reduce the risk of infections in individuals with compromised immune function.
3. Supportive Care and Infection Prevention: Maintaining good hygiene practices, avoiding exposure to infectious agents, and practicing infection prevention measures are essential for individuals with leukopenia. This includes frequent handwashing, avoiding crowded or high-risk environments, staying up-to-date with vaccinations (as recommended by healthcare providers), and promptly seeking medical attention for any signs of infection.
4. Blood Transfusions: In severe cases of leukopenia associated with significant blood loss, anemia, or impaired coagulation, blood transfusions may be necessary to replenish white blood cells and other blood components. Transfusions of packed red blood cells, platelets, or fresh frozen plasma may be administered based on individual needs and clinical indications.
5. Nutritional Support: Optimizing nutritional intake and addressing deficiencies in vitamins, minerals, and macronutrients can support immune function and white blood cell production. Healthcare providers may recommend dietary changes, oral supplements, or intravenous nutrition (parenteral nutrition) to address specific nutrient deficiencies and promote overall health.
6. Monitoring and Follow-Up: Regular monitoring of white blood cell counts, clinical symptoms, and response to treatment is essential for managing leukopenia effectively. Healthcare providers may perform periodic blood tests, physical examinations, and imaging studies to evaluate disease progression, treatment response, and potential complications.
V. Lifestyle Modifications and Home Care for Leukopenia

1. Diet and Nutrition: A balanced diet rich in vitamins, minerals, antioxidants, and protein is essential for supporting immune function and white blood cell production. Emphasize foods high in vitamin C (citrus fruits, berries, bell peppers), vitamin E (nuts, seeds, vegetable oils), vitamin A (carrots, sweet potatoes, leafy greens), zinc (lean meats, seafood, nuts, seeds), and iron (lean meats, legumes, fortified cereals) to promote immune health.
2. Hygiene Practices: Maintaining good hygiene habits can help reduce the risk of infections in individuals with leukopenia. Wash your hands frequently with soap and water, especially before eating, after using the restroom, and after touching surfaces in public places. Avoid close contact with individuals who are sick, and cover your mouth and nose with a tissue or your elbow when coughing or sneezing.
3. Environmental Precautions: Minimize exposure to environmental toxins, pollutants, and chemicals that may impair immune function or exacerbate leukopenia. If you work in environments with potential hazards (such as construction sites, industrial facilities, or agricultural settings), use appropriate protective equipment (such as masks, gloves, and goggles) and follow safety guidelines to reduce exposure risks.
4. Stress Management: Chronic stress can weaken the immune system and exacerbate leukopenia symptoms. Practice stress-reduction techniques such as deep breathing exercises, meditation, yoga, progressive muscle relaxation, or mindfulness to promote relaxation and enhance immune resilience. Engage in activities that promote mental and emotional well-being, such as hobbies, socializing with loved ones, and spending time in nature.
5. Exercise and Physical Activity: Regular exercise can boost immune function, improve circulation, and enhance overall health and well-being. Aim for at least 30 minutes of moderate-intensity aerobic activity (such as brisk walking, cycling, or swimming) most days of the week, supplemented with strength training exercises to build muscle mass and support immune health. Consult with your healthcare provider before starting any new exercise regimen, especially if you have underlying health conditions or concerns.
VI. Coping Strategies and Support for Individuals with Leukopenia
1. Education and Self-Advocacy: Educate yourself about leukopenia, its causes, symptoms, and treatment options. Take an active role in your healthcare by asking questions, seeking information from reliable sources, and advocating for your needs and preferences. Work collaboratively with your healthcare team to develop a personalized treatment plan that addresses your unique circumstances and goals.
2. Support Networks: Seek support from family members, friends, and support groups who understand your condition and can provide emotional support, encouragement, and practical assistance. Connect with online communities, forums, or social media groups dedicated to individuals living with leukopenia or related immune disorders to share experiences, insights, and coping strategies.
3. Mental Health and Well-Being: Living with a chronic health condition like leukopenia can take a toll on your mental and emotional well-being. Practice self-care activities that promote relaxation, stress reduction, and emotional resilience. Engage in hobbies, interests, and activities that bring you joy and fulfillment, and prioritize activities that nourish your mind, body, and spirit.
4. Healthcare Communication: Maintain open and honest communication with your healthcare providers about your symptoms, concerns, and treatment preferences. Be proactive in reporting any changes in your condition, adverse effects of medications, or new symptoms that may arise. Work together with your healthcare team to address any challenges or obstacles you may encounter along your healthcare journey.
5. Long-Term Planning: Develop a long-term plan for managing leukopenia and maintaining your overall health and well-being. Discuss with your healthcare provider the potential implications of leukopenia on your daily life, work, relationships, and future goals. Explore strategies for mitigating risks, optimizing treatment outcomes, and planning for potential complications or changes in your health status over time.
VII. Conclusion: Empowering Individuals Living with Leukopenia
In conclusion, leukopenia is a complex medical condition that requires comprehensive evaluation, personalized treatment, and ongoing management to optimize outcomes and quality of life. By understanding the causes, symptoms, and treatment strategies for leukopenia, individuals can take proactive steps to protect their immune health, reduce infection risks, and enhance overall well-being. With the support of healthcare providers, caregivers, and support networks, individuals living with leukopenia can navigate the challenges of their condition with resilience, empowerment, and hope for the future.
This comprehensive guide provides a detailed overview of leukopenia, covering its causes, symptoms, diagnosis, treatment strategies, lifestyle modifications, coping strategies, and support resources. By addressing leukopenia from a holistic perspective and empowering individuals with knowledge and insights, we aim to improve outcomes and enhance the quality of life for those affected by this condition. For More Information you can check our blogs “Understanding HIV/AIDS: Advances, Challenges, and Hope for the Future”.
